Free Progress Notes Template
The Progress Notes form is an essential tool in the medical record-keeping process, designed to capture vital information about a patient's care and treatment over time. This standardized document includes key details such as the date of the entry, the patient's identification, and the medical facility where the care is provided. It requires the patient's name, including last, first, and middle initials, along with their grade, rank, and rate. Additionally, the form includes a unique register number and ward number to ensure accurate tracking and organization within the medical records system. By documenting each patient's progress, healthcare providers can create a comprehensive overview of the patient's condition, treatment plans, and any changes in health status. This form, identified as Standard Form 509, has undergone revisions to maintain its effectiveness and relevance in medical practice, ensuring that healthcare professionals can provide the best possible care based on up-to-date information.
Document Specifics
| Fact Name | Description |
|---|---|
| Form Title | The form is officially titled "Medical Record Progress Notes." It is used to document patient care and treatment progress. |
| Governing Authority | This form is prescribed by the General Services Administration (GSA) and the Information Collection Management Regulations (ICMR), as outlined in 41 CFR 201-9.202-1. |
| Revision Date | The current version of the form is a revision dated July 1991 (REV. 7-91). |
| Patient Identification | Patients must be identified by their last, first, and middle names, along with their grade, rank, rate, and the medical facility they are associated with. |
| Registration Information | The form requires a registration number and a ward number to facilitate proper tracking and documentation. |
| Usage | Progress notes are essential for documenting ongoing patient care, treatment updates, and any changes in the patient's condition. |
| Continuation | There is a provision for continuation on the reverse side of the form, allowing for additional notes if necessary. |
Similar forms
The Progress Notes form is similar to several other documents used in medical records. Each serves a unique purpose while maintaining a focus on patient care and documentation. Below are four documents that share similarities with the Progress Notes form:
- Patient Intake Form: This document collects essential information about the patient, including personal details and medical history. Like Progress Notes, it is vital for creating a comprehensive understanding of the patient's background and needs.
ATV Bill of Sale: This document is essential for the sale of all-terrain vehicles in California, capturing key details about the transaction. For more information and to access the form, visit California PDF Forms.
- Clinical Summary: A Clinical Summary provides an overview of the patient’s treatment and progress over time. Similar to Progress Notes, it highlights key developments in the patient’s condition and outlines future care plans.
- Discharge Summary: This document is completed when a patient is discharged from care. It summarizes the treatment received and the patient's status at discharge, akin to Progress Notes, which document ongoing patient care and progress.
- Medication Administration Record (MAR): The MAR tracks medications administered to the patient. It shares a focus on patient safety and treatment, just as Progress Notes do, by documenting specific actions taken during the patient’s care.
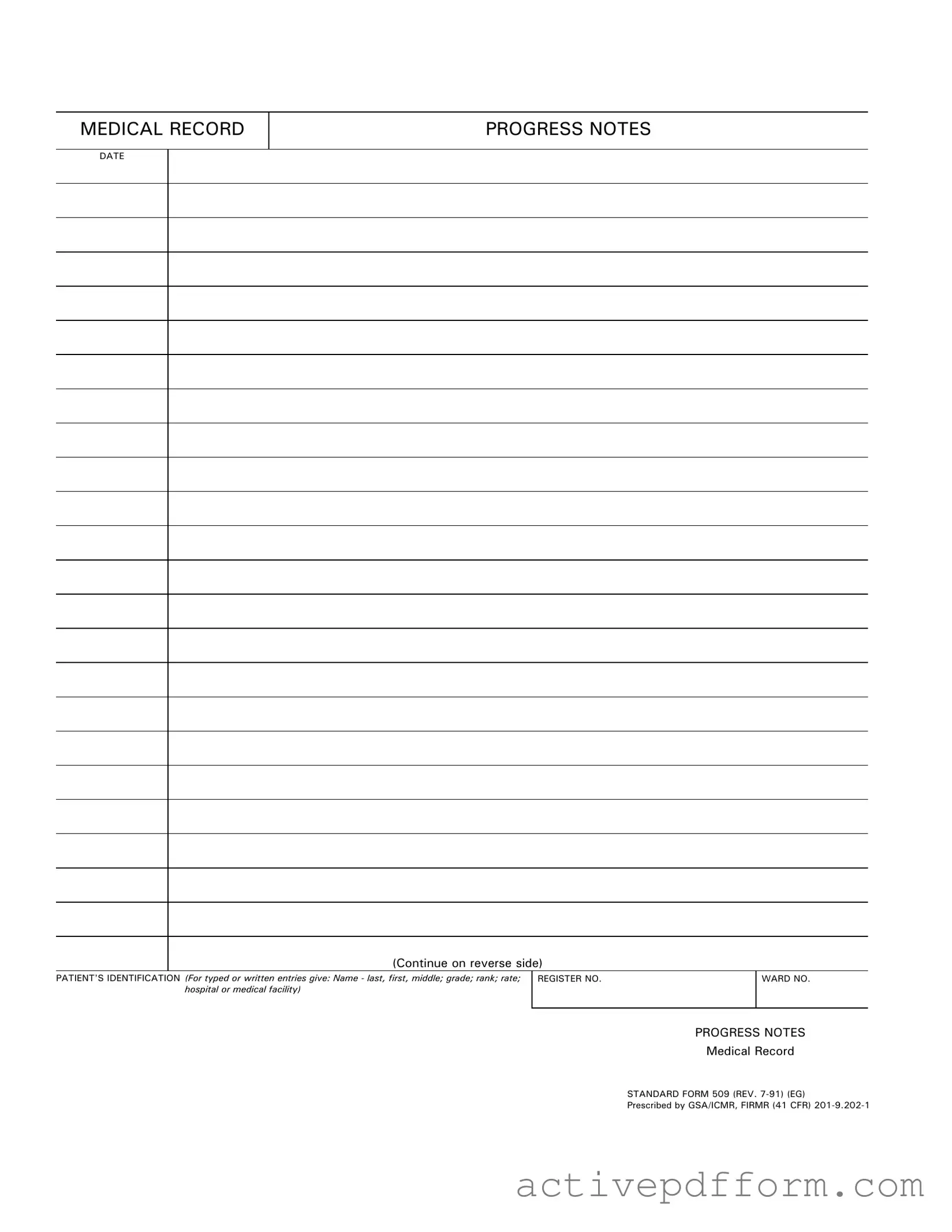
Progress Notes Example
MEDICAL RECORD
PROGRESS NOTES
DATE
(Continue on reverse side)
PATIENT'S IDENTIFICATION (For typed or written entries give: Name - last, first, middle; grade; rank; rate; hospital or medical facility)
REGISTER NO. |
WARD NO. |
|
|
PROGRESS NOTES
Medical Record
STANDARD FORM 509 (REV.
Prescribed by GSA/ICMR, FIRMR (41 CFR)
PROGRESS NOTES
DATE
STANDARD FORM 509 (REV.
Understanding Progress Notes
What is the purpose of the Progress Notes form?
The Progress Notes form is designed to document a patient's ongoing medical care and treatment. It provides a structured way for healthcare providers to record observations, treatments, and any changes in a patient's condition over time. This ensures continuity of care and helps keep all members of the healthcare team informed.
What information is required on the Progress Notes form?
When filling out the Progress Notes form, you need to include several key details. This includes the patient's identification information, such as their name (last, first, middle), grade, rank, rate, and the medical facility or hospital where they are receiving care. Additionally, the date of the notes should be clearly indicated to track the timeline of the patient's treatment.
How should I fill out the patient's identification section?
In the patient's identification section, provide the full name of the patient in the specified order: last name, first name, and middle name. Include their grade, rank, and rate if applicable. This information helps ensure that the records are accurately attributed to the correct individual, which is crucial for effective medical care.
Can I continue writing on the reverse side of the Progress Notes form?
Yes, if you require more space for your notes, you can continue writing on the reverse side of the Progress Notes form. This allows for a more detailed account of the patient's progress and any additional observations that may be necessary for comprehensive documentation.
What is the significance of the date on the Progress Notes form?
The date on the Progress Notes form is essential for tracking the timeline of a patient's treatment and progress. It helps healthcare providers reference specific events and changes in the patient's condition over time. Accurate dating also plays a critical role in ensuring compliance with medical record-keeping regulations.
Who is responsible for completing the Progress Notes form?
The healthcare provider who is directly involved in the patient's care is responsible for completing the Progress Notes form. This may include doctors, nurses, or other medical staff. It is important that the person filling out the form is familiar with the patient's case to provide accurate and relevant information.
Is there a specific format that must be followed when writing notes?
While there is no strict format mandated, it is important to write notes clearly and concisely. Use professional language and ensure that all entries are legible. If abbreviations are used, they should be widely recognized in the medical field to avoid confusion. Consistency in documentation helps maintain clarity and effectiveness in patient care.
What happens if I make a mistake on the Progress Notes form?
If you make a mistake on the Progress Notes form, it is important to correct it properly. Cross out the error with a single line, and initial and date the correction. This maintains the integrity of the medical record while providing a clear audit trail of changes made. Avoid using correction fluid or erasers, as this can lead to confusion about the original entry.
Dos and Don'ts
When filling out the Progress Notes form, there are important things to keep in mind. Here’s a list of what you should and shouldn't do:
- Do write clearly and legibly.
- Do include the patient's full name and identification details.
- Do use the correct date for each entry.
- Do follow the standard format provided on the form.
- Do keep your notes concise and relevant.
- Don't leave any sections blank unless instructed.
- Don't use abbreviations that are not widely recognized.
- Don't alter the form in any way.
- Don't include personal opinions or unnecessary information.
- Don't forget to review your notes for accuracy before submission.
Check out Common Templates
Insurance Card Maker - Ensure you know how to contact your insurance company in an emergency.
The Nyc Apartment Registration Form is an essential document for landlords and property managers in New York City. This form collects important information about the apartment and its owner, helping to ensure compliance with housing regulations. For those looking for a streamlined approach in filling out this form, you can access a helpful resource at https://nytemplates.com/blank-nyc-apartment-registration-template. Properly completing and submitting this form is crucial for facilitating the rental process and maintaining transparency.
Da - The form includes a reverse side for additional inventory if needed.
Dd Form 2656 March 2022 - This document helps the Department of Defense track retiree paycheck distributions.